Intrastromal Ablation for the Correction of Presbyopia in Human Eyes
March 19, 2009
In an interview with Cataract & Refractive Surgery Today (October 2008 Issue), Frieder Loesel, General Manager of 20/10 Perfect Vision, following the announcement that his company had formed a joint venture with Bausch & Lomb focused solely on the laser refractive market, stated that the new company, Technolas Perfect Vision, would investigate laser-based treatments for presbyopia, including intrastromal ablation (ISA). That statement piqued my interest, since I have been involved with the concept of ISA since my earliest involvement with ophthalmic lasers beginning in the mid-1980s. I decided that the research being conducted by Technolas Perfect Vision might just lead, finally, to a successful conclusion to the search for the “home run” using this technique.
In this report, I would like to tell you about the technology of ISA, its history, and the results of the latest experiments being done by Dr. Luis Ruiz on behalf of 20/10 Perfect Vision (about to become Technolas Perfect Vision).
What is ISA?
Intrastromal ablation is the use of a focused laser beam to create a plasma in tissue which, when it expands, causes a shock wave, transforming into an acoustic transient, all resulting in a cavitation bubble which, upon collapse leaves behind a gas bubble containing carbon dioxide and other gases and a space. By using a tiny spot size and moving the laser focus within the cornea, an area of tissue can be accurately removed. Using this technique within the corneal stroma, and with the collapse of the upper layer of tissue above the gas bubble (with the absorption of the gases) onto the bottom layer, the shape of the cornea can be changed.
This technology is fully explained by the following figures taken from an article by Jay Pepose and Holger Lubatschowski, appearing in the October 2008 issue of Cataract & Refractive Surgery Today (1) . (Used with permission of the authors and the publisher.)
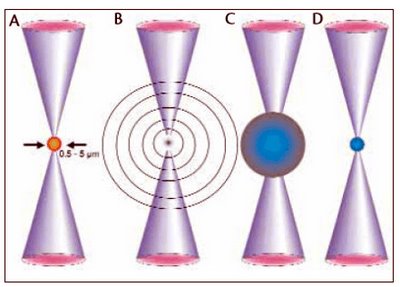
Figure 1. The course of a photodisruptive process is shown.
Due to multiphoton absorption in the focus of the laser beam, a plasma develops (A). Depending on the laser parameters, the diameter varies between 0.5 ?m to several micrometers. The expanding plasma drives as a shock wave, which transforms after a few microns to an acoustic transient (B). In addition to the shock wave’s generation, the expanding plasma has pushed the surrounding medium away from its center, which results in a cavitation bubble (C). The maximum diameter of the cavitation bubble can reach 10 to 100 ?m. Its lifetime is only a few microseconds. After the collapse of the cavitation bubble, a gas bubble (and space) is left behind, containing carbon dioxide and other gas molecules (D).
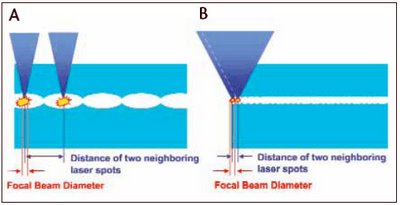
Figure 2. Tissue Removal
Higher pulse energy (A) allows the use of greater spacing between spots, because the cutting process is driven primarily by expanding cavitation and residual gas bubbles. Lower pulse energy (B) and smaller spot size and volume require substantially more spots with tighter spacing and greater overlap, as the cutting process here is driven primarily by the plasma itself. To deliver this many spots in a reasonable time frame requires a very-high-frequency engine.
The question remaining is: Can this tissue removal be done accurately and predictably enough to facilitate a pre-determined change in corneal shape?
In his latest paper (2) describing IntraCOR, the Intrastromal ablation for correcting presbyopia, Dr. Luis Ruiz says, “By means of the femtosecond laser, a customized pattern is applied into the cornea inducing a focal reorganization of the biomechanical fores. In dependence of the applied pattern, the corneal surface can be locally flattened or steepened”.
What Dr. Ruiz states may be so, but it still doesn’t answer the question posed above – can this technique result in a controllable, predictable result. We will just have to wait and see if the use of the femtosecond laser can do what others with other laser systems have tried and failed to do in the past.
The History of ISA
Automated Laser Systems
My involvement with ophthalmic lasers dates back to 1983, when I wrote a paper titled, “The Outlook for Lasers in Ophthalmology” for Decision Resources, a subsidiary of Arthur D. Little (ADL). This was shortly after the first lasers for use in ophthalmology were granted FDA approval.
In order to keep up with this emerging technology, I had begun to attend the annual meetings of the American Academy of Ophthalmology (AAO). At the 1985 AAO Meeting, I discovered a new, interesting company called Automated Laser Systems (ALS). This company had developed a finely focused, pulsed, excimer-pumped dye laser, the CALM 1000 (Computer Aided Laser Microsurgery), operating at 595 nm, that it claimed was capable of producing micro bursts of energy within the corneal stroma to ablate stromal tissue with an extremely small (5-10 microns) surrounding tissue damage zone. At the meeting, the company was demonstrating the laser by engraving clear, one-half inch diameter corneal-shaped acrylic discs with patterns within the center of the disc. I still have two of the patterned discs and have attempted to show the engraved patterns in the photographs below:

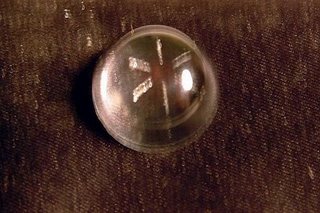

Photos taken of laser engraved acrylic discs using the ALS CALM 1000 laser, Fall 1985.
As I later learned, the ALS program ran out of funds and never completed its development program.
Phoenix Laser Systems
In August, 1989, I was retained by a new startup laser company, Phoenix Laser Systems, to produce a technology overview report of the ophthalmic laser workstation that they had developed, whose primary aim was to use intrastromal ablation for correcting vision. It turned out that the principals of Phoenix Laser, Steve Schiffer and Alfred Sklar, were also involved in starting up Automated Laser Systems, but they had severed their ties with ALS prior to forming Phoenix.
The Phoenix Laser Workstation was composed of a unique imaging and diagnostic system, along with a pulsed doubled YAG laser for performing intricate and precise laser tissue removal within the corneal stroma.
Over a period of several months, my colleague Ken Taylor and I visited the Phoenix laboratory facility, located near the Lawrence Livermore National Laboratories, and their corporate offices in San Francisco. We interviewed the principals and their staff of scientists and engineers, collected information about potential competitors, and assessed the market for their device. This culminated in a report, prepared in March 1990, titled, “Technology Overview: Phoenix Laser Systems”.
In September 1990, Ken Taylor and I, along with other colleagues from ADL, prepared an updated Technology Overview report. The updated report contained our assessment of the future potential for the Phoenix Ophthalmic Workstation, based on forecasted markets for specific applications. In addition, we reviewed and observed the initial animal and human clinical trials conducted with the Phoenix system.
I won’t go into detail about our forecasted market potential, but would like to briefly discuss the results of the first animal and human clinical trials observed by Dr. Taylor at the Barraquer Institute in Bogota, Columbia. The trials were supervised by Dr. Carmen Barraquer and Alfred Sklar, Director of R&D for Phoenix. (Interestingly, the Phoenix Laser system was set up in the former office space of Dr. Luis Ruiz, who had left the Barraquer Institute to start up his own ophthalmic institute in Bogota.)
The following passages are taken from our September 1990 report:
Animal Studies
Once optimal laser settings were established with the rabbit eyes, intrastromal ablations were performed and it was shown that the formed bubbles dissipated and were absorbed within 30 minutes. No trace of the lesions, except for a faint haze, could be seen within the following 24-48 hours, after which, even the trace haze was invisible to slit lamp investigation.
Intrastromal lesions placed in the anterior stroma caused significant flattening of the corneal surface above the lesions, which stabilized between 12-24 days postoperatively. No damage to descemet’s membrane or to endothelium cells was observed.
Human Eye Results
Just prior to Dr. Taylor’s arrival in Bogota, eight human non-sighted eyes were treated with intrastromal ablations. Dr. Taylor had the opportunity to review the case histories and evaluate two of the patients postoperatively. The patients reported no pain or foreign body sensations in their eyes and the corneas and all tissues in the region of the lesions remained clear. Neither the operating physician nor the observers were able to see the lesion edge two days postoperatively.
Flattening of the cornea was determined and the enucleated eyes were scheduled for histopathological examination at either Wilmer Eye Institute at Johns Hopkins or at the Barraquer Institute.
Over the following months, the Arthur D. Little team continued to be in touch with the principals at Phoenix Laser. However, I began asking searching questions about the clinical results, similar to what I have proposed in the beginning of this article, and soon was told my services were no longer needed.
Dr. Taylor continued to work for Phoenix for a few months more until, as with the predecessor company, ALS, funds were no longer available to support the company’s efforts.
It is my understanding that the company was never able to produce reliable and predictable results.
Intelligent Surgical Lasers (ISL)
At about the same time that the developmental work on ISA was underway at Phoenix Laser Systems in San Francisco, another California company was also conducting research in the use of a laser for ISA. This was Intelligent Surgical Lasers, located in San Diego and founded in December 1987 by Josef Bille, formerly of Heidelberg Engineering, and Dr. Stuart Brown of La Holla, CA.
I was impressed by the company’s initial showing at an AAO Meeting probably in 1989. At the meeting, it unveiled its model 2001 MPL picosecond, microjoule, diode-pumped YLF laser which it claimed could be operated at either 1053 nm, or doubled to 527 nm, thus allowing both photodisruption and photocoagulation.
In November 1989, and again in June 1990, I was asked by two investment firms to undertake a technical evaluation of ISL, similar to what had been done with Phoenix. However, the principal investment partner, H&Q Life Science Technology Fund, and its General Partner Robert Kunze refused to allow me to become involved with the company, and I was never provided access to any of the results obtained with its technology, other than from papers delivered at public ophthalmic meetings.
I can only assume that its picosecond laser was not successful in performing reliable and reproducible intrastromal ablations, as the company eventually lost its funding and merged with another company, Escalon Medical (see below).
Interestingly, Josef Bille went on to become a founder of another company pursuing the dream of intrastromal ablation, 20/10 Perfect Vision!
The Femtosecond Laser Companies and ISA
University of Michigan and IntraLase (now part of AMO)
In March 1994, I became involved with femtosecond lasers. I was hired by the University of Michigan to help them assess the commercial opportunities for their ultra-fast laser technology, developed by Ron Kurtz and his associates at the Ultra Fast Laser Center. After spending a day with representatives of the University Technology Management Office, the Ultrafast Optical Science division, and Dr. Kurtz from the W.K. Kellogg Eye Center, I prepared a several page report providing them my thoughts of what the ultra-fast lasers might be commercially capable of and for “hitting a home run” – which I said was refractive surgery via intrastromal ablation, if they could pull it off.
In July, 1997, the University of Michigan’s Technology Management Office announced the spin-off of Intralase Corporation, a startup company that would develop and commercialize novel ultra-fast laser technology, beginning in the ophthalmic field. The announcement mentioned an expected collaborative industrial relationship with an industry participant, which was in negotiation. That negotiation turned out to be with Escalon Medical, who had acquired the assets of Intelligent Surgical Laser, including its patent portfolio in a reverse buyout in February 1996.
As it turned out, Intralase concentrated its efforts with its femtosecond laser on creating flaps for LASIK surgery, and have been very successful in this effort, much to my surprise. I once wrote that I didn’t think many ophthalmologists would pay the high price of $350,000 for a laser microkeratome! Obviously, I was proven wrong.
During the late 1990s, I attended several presentations and wrote about doctors involved with IntraLase discussing their research on the use of the femtosecond laser for performing intrastromal ablation. Perhaps, the company is still conducting such research.
In addition to the IntraLase FS (the current version of the IntraLase laser) from Advanced Medical Optics (AMO), there are at least three other femtosecond lasers on the market – the Femtec from Technolas Perfect Vision; the VisuMax from Carl Zeiss Meditec; the Femto LDV from Ziemer Ophthalmic Systems Group; and at least one more in development from a startup group of former IntraLase scientists at a company called LensX in Aliso Viejo, CA.
For complete information about the four commercially available femtosecond lasers, please see the two articles in the October 2008 issue of Cataract & Refractive Surgery Today. The first, from Jay Pepose and Holger Lubatschowski titled: “Comparing Femtosecond Lasers”(1), while the second written by Perry Binder is titled: “Femtosecond Lasers: How do you select a system”(3).
IntraCOR Intrastromal Ablation for Correcting Presbyopia
As I mentioned up front, the reason this article was written is because I became aware of the work being done by Dr. Luis Ruiz of Bogota, Columbia on behalf of 20/10 Perfect Vision (soon to be Technolas Perfect Vision), on using intrastromal ablation for the correction of presbyopia in human eyes.
I would just like to comment briefly on Dr. Ruiz’s latest paper, taken from the 20/10 Perfect Vision website (2).
As reported by Dr. Ruiz, his paper summarizes the worldwide first, still preliminary clinical results of an ongoing pilot study concentrating on non-invasive, intrastromal correction of presbyopia, performed by means of a FEMTEC femtosecond laser system from 20/10 Perfect Vison of Heidelberg, Germany.
The general purpose of the study was to quantify the feasibility of non-invasive intrastromal corrections of ametropic eyes, with the first phase focused on the correction of presbyopia.
More than 200 presbyopic eyes underwent intrastromal refractive surgeries with the FEMTEC femtosecond laser, with all treatments performed at the Centro Oftalmologico Colombiano in Bogota, starting in October 2007.
Depending on the refractive properties, as well as on the individual biomechanical and geometrical properties of the cornea, a customized pattern for each eye was calculated, supported by Finite Element Modeling, and the intrastromal laser treatment was performed with treatment times between 18 and 30 seconds. The treatment was done in the mid-stroma, so as to not allow for an anterior or posterior surface incision, hence significantly reducing the risk of healing issues.
The following figures and graphs are reproduced with permission of the author.)
The Finite Element Modeling using a spatial 3D grid adapted to the individual curvature of the cornea is illustrated in the following sketch:
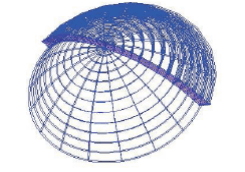
Fig. 3: 3D Sketch of corneal Finite Element Modeling model used for the calculation of individual treatment patterns
While the customized intrastromal treatment pattern is shown below:
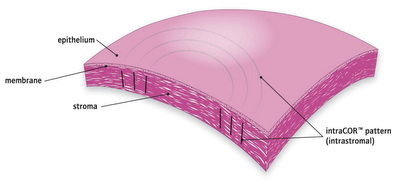
Fig. 4: Sketch of customized intrastromal treatment pattern
In general, the patients showed an increase in Near UCVA within minutes to a few hours of treatment. The induced increase was found to be stable within the observed follow-up time of up to 11 months, as shown in the graphs below:
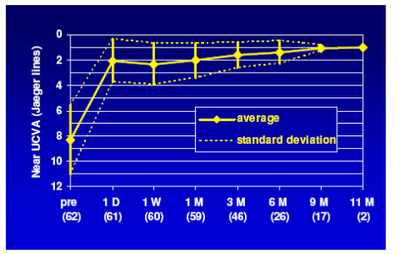
Fig. 5: Efficacy and stability: Near UCVA change after intrastromal correction of presbyopia
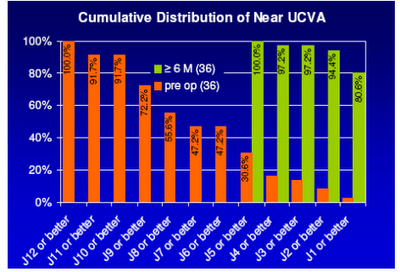
Fig. 6: Refractive outcome distribution of Near UCVA according to Jaeger readings, pre-op and after the maximum observation period of at least 6 months
An important consideration is the factor of safety. Any approach to improving near vision is only viable if the Distance UCVA and Distance BSCVA are either unaffected or, at worst, only minimally affected.
The graphs below show the Cumulative Distribution of Distance UCVA and the distribution of Distance BSCVA following treatment:
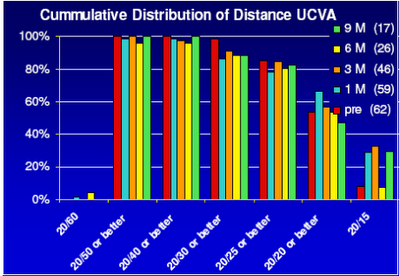
Fig. 7: Cumulative distribution of Distance UCVA of patients undergoing intrastromal presbyopia correction
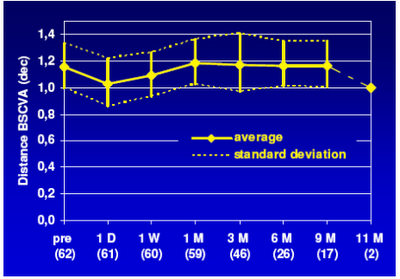
Fig. 8: Cumulative distribution of Distance BSCVA of patients undergoing intrastromal presbyopia correction
In summary, the preliminary results of the ongoing clinical study show an average gain of 6.2 +/- 2.8 Jaeger lines is achieved in Near UCVA after 3 months postop, by inducing only minor effects on the Distance UCVA.
As Dr. Ruiz concludes, “The promising initial results will need to be further supported by a larger number of procedures performed at several clinical sites in the near future. Parallel to the very successful investigation of intrastromal presbyopia correction, further treatment strategies for non-invasive correction of other forms of ametropia (myopia, hyperopia, astigmatism) are currently under investigation. The preliminary results of these treatments are equally promising for using the FEMTEC laser system for all kinds of such intrastromal corrections.”
So, it seems that perhaps the dream of intrastromal ablation may have found a solution. However, being the skeptic I am, I will await further proof before accepting the premise.
References:
1.”Comparing Femtosecond Lasers”, Pepose & Lubatschowski, Cataract & Refractive Surgery Today, October 2008, pgs 45-52.
2. “Preliminary clinical results with 11-months follow-up of intrastromal correction of presbyopia (IntraCOR) using the FEMTEC femtosecond laser system”, 20/10 Perfect Vision website, October 2008.
3. “Femtosecond Lasers: How do you select a system”, Binder, Cataract & Refractive Surgery Today, October 2008, pgs 53-56.
Reprinted with permission of Irv Arons (originally published on Irv Aron’s Journal).
Comments
Jump down to form below to submit your own comments
3 Responses to “Intrastromal Ablation for the Correction of Presbyopia in Human Eyes”
Dave,
The new leader in the field is 20/10 Perfect Vision (and the joint venture with B&L).
That’s the direction to look for the future.
Irv Arons
Very interesting and exciting technology. I wonder what will happen to it now that AMO has been purchased?
Sincerely,
David D. Richardson, M.D.?
Medical Director
San Gabriel Valley Eye Associates, Inc. ?
207 S. Santa Anita Street, Suite P-25 ?
San Gabriel, CA 91776 ?
626.289.7856


